The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot
Table of Interests
Today, you and I will quickly take a look at the topic “The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot“.
This has become necessary as we have sen overtime that several individuals have been searching for topics related to the above topic The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot.
However, if you are among those that have been searching for answers to [blue baby syndrome definition, blue baby syndrome symptoms, blue baby syndrome pictures, blue baby syndrome is caused by the contamination of, blue baby at birth, blue baby syndrome blood type, what is the most common cause of a blue baby?, blue baby ghost, The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot], then you can see that you are not the only one.
Nonetheless, you shall get all this information right here on this blog.
The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot

Today, we’re going to talk about the Tetralogy of Fallot, a set of congenital heart defects which could cause serious complications without appropriate interventions. Some of you might have heard about the Blue Baby Syndrome before, and I must clarify, it does not specifically refer to the Tetralogy of Fallot.
The Blue Baby Syndrome refers to any conditions usually related to heart or blood which could potentially lead to cyanosis, a condition whereby the skin or mucous membrane of an individual turns blue as a result of poor oxygen saturation or inability for the blood in the circulation to fulfill the body’s demand for oxygen.
Cyanosis can simply be divided into two which are central and peripheral. In medical school, I was taught on how to check for either of these condition through a thorough physical examination.
Peripheral cyanosis usually refers to any bluish discoloration of the distal compartment (hands or feet) and central cyanosis can usually be examined around the lips or tongue.
Pretty simple right? Theoretically, yes, but clinically, patients might present with a different set of symptoms which could indicate they were in the state of hypoxia (reduced oxygen saturation in the blood); that’s why clinical experience is of utmost importance in making an accurate clinical diagnosis.
As the name indicates, the Tetralogy of Fallot (TOF) consists of 4 kinds of cardiac-related pathologies which are:

A) Subpulmonary stenosis
B) Overriding aorta
C) Ventricular septal defect (VSD)
D) Right ventricular hypertrophy
Even though this condition can lead to serious sequelae, the mortality rate of patients who were born with TOF is quite low. If you want to talk about the life expectancy of patients with TOF 30 years ago, most of them (approximately 85%) survived to their 40s; some even gave birth to a few babies which signifies that the medical care for this condition has been great since then. Nowadays, the field of medicine has advanced significantly compared to the last 30 years and the quality of life of individuals with cyanotic heart diseases have improved. This is attributable to the advanced of medical and surgical management which leads to a deeper understanding of the pathological aspect of diseases and its potential cure.
The ventricular septal defect

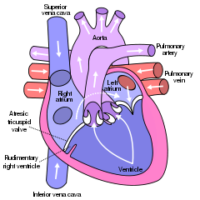
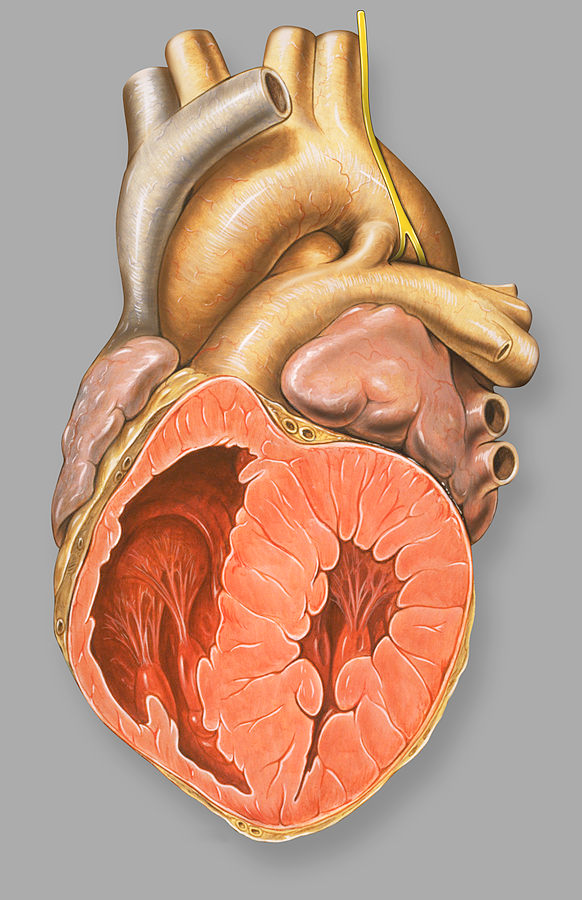
The ventricular septal defect (VSD) is a fancy term for a hole in the wall of the ventricle of the heart. I’m not going to outline the overall anatomy of the heart but what you need to know is, a heart is made up of 4 chambers.
All of the chambers were working hard to pump blood either to the lungs to be reoxygenated or to the systemic circulation, supplying every single cell in the body with oxygen.
Atria would serve as the entry point and ventricles as the resting chamber before the blood would be pumped out.
Both of the atria would be separated by a muscular wall called the interatrial wall while ventricles would be separated from each other by the interventricular wall. I think by now you already knew that the ventricular septal defect describes a hole in the inter ventricular septum (wall).
This hole will result in the mixing of blood from the systemic and pulmonary (related to lungs) circulation causing the oxygenated and de oxygenated blood to mix.
As a result, the oxygenated blood portion which is pumped to the systemic circulation reduces making oxygen delivery less effective. There are two types of VSD which are:

- Muscular (affect the part of the ventricular wall which is filled with muscle)
- Perimembranous (affect the part of the ventricular wall which is adjacent to the tricuspid valve)
The severity of a VSD is often correlated to the size of the hole which caused blood to flow from the left chamber into the right chamber (due to the pressure difference).
Either it is large or small would be determined by its size relative to the aortic opening. If the size of the inter ventricular septal is larger than the size of the aortic opening, then it is a large defect.
Otherwise, it would be considered as a small defect. Patients with a small VSD were often asymptomatic, most of them only will become symptomatic if there are other external factors which affect their energy consumption i.e. rigorous exercise, infection or pregnancy.
Overriding aorta, sub-pulmonary obstruction, and right ventricular hypertrophy
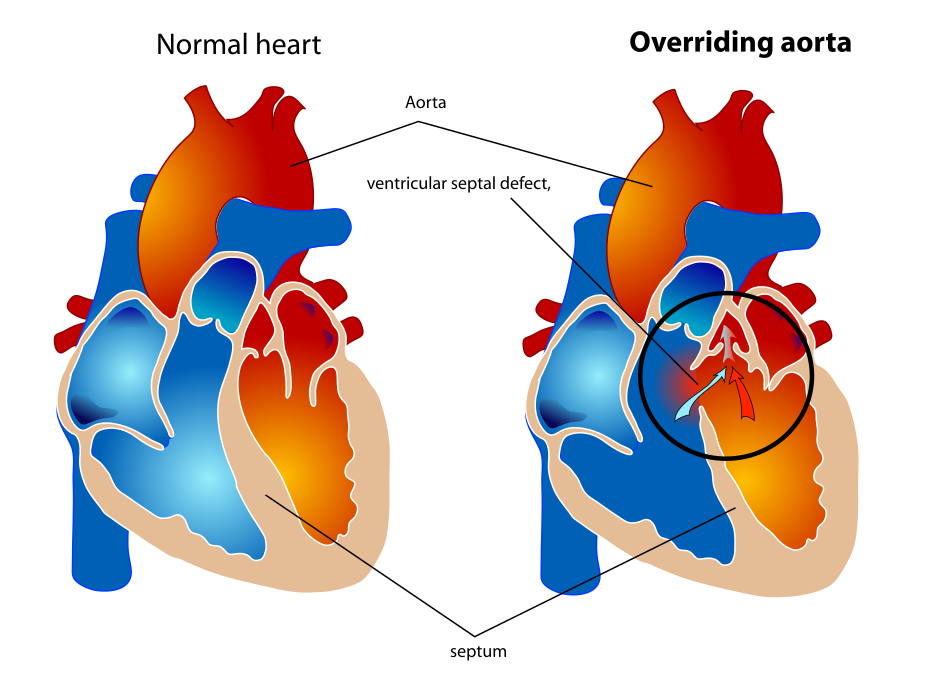
In a normal, healthy individual, the aorta would be the entry point of the oxygenated blood into the systemic circulation.
In patients with TOF, the most common type of VSD would be the perimembranous type.
A wall defect adjacent to the tricuspid valve provides an opening for the deoxygenated blood to pass through allowing them to be pumped into the systemic circulation.
So why is it the blood from the right side of the heart can be pumped into the aorta considering the amount of pressure in the left side of the heart is higher than the right side of the heart?
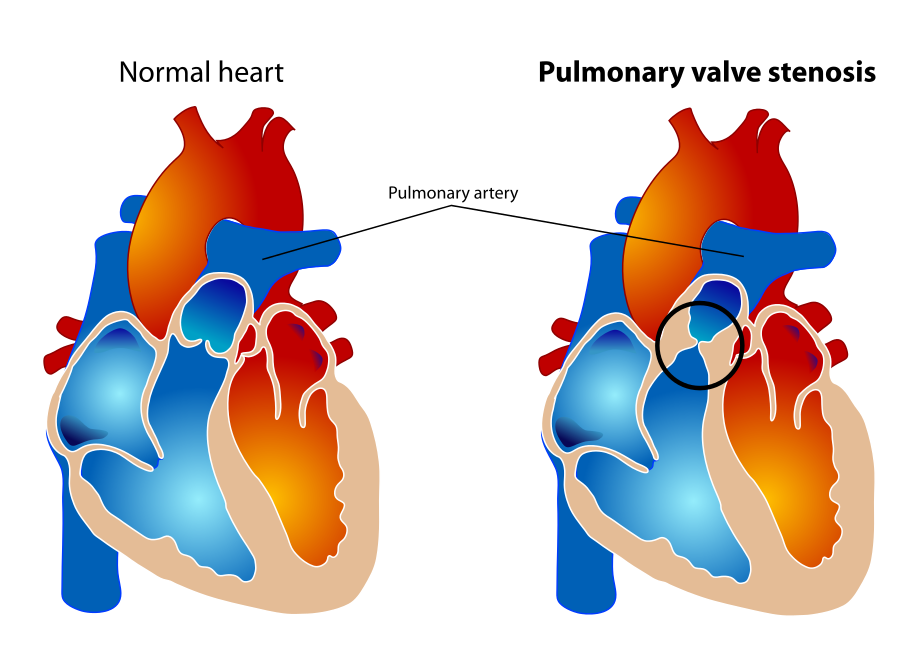
This is because, in patients with TOF, they will also present with sub-pulmonary obstruction, which affects the pulmonary artery.
All of the arteries in the body would carry oxygenated blood except for pulmonary artery; that was the rule of thumbs that have been taught in the medical school over and over again.
The pulmonary artery will bring the deoxygenated blood into the pulmonary circulation to be oxygenated.
The obstruction or narrowing was caused by various anatomical abnormalities in the trabeculae of the heart septum causing it to become narrow.
This will lead to an accumulation of blood in the right ventricle caused by the obstruction hence, right ventricular hypertrophy (increased in size of the right ventricle).
As the volume increases, the pressure rises. This will cause the deoxygenated blood in the right ventricle to be “accidentally” pumped through the septal defect, into the aorta and finally, the systemic circulation.
The Role Of Ductus Arteriosus In The Tetralogy Of Fallot
That’s it, all of the components of the tetralogy have been explained.
Most of the patients who were admitted to the hospital for TOF are neonates (between 0-28 days old) but then again it will depend on the severity of the defect.
Some of the patients admitted to the hospital later when they were starting to show signs and symptoms of cyanosis associated with some respiratory distress.
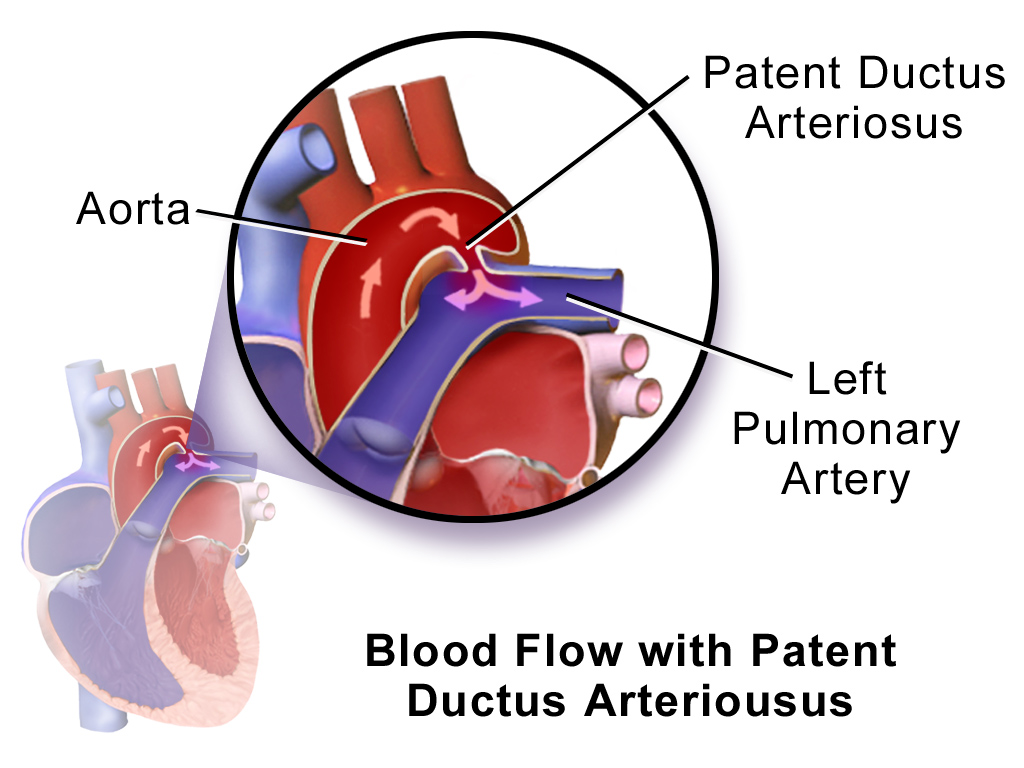
The reason why babies who were born were not hypoxic even with the heart defects is due to the fact that, there is a connection between the pulmonary artery and the proximal descending aorta. This connection was called ductus arteriosus.
Ductus arteriosus is a fetal blood vessel which will bypass the non-functioning fetal lungs to supply the other organs during infancy.
In a normal individual, the ductus arteriosus will be completely closed after 2-3 days of life.
It has to be closed to prevent blood flowing from the aorta into the pulmonary circulation causing signs and symptoms which resembles patients who were diagnosed with a VSD (It’s a left to right shunt).
There are two major factors which would cause the connection to close:
See Other Articles People Are Reading
- Cry Me A River – From Biology To Psychology Of Tears
- Redefining ‘Health’ For The 21st Century | Health Care Changes In The 21st Century
- Missile Technology – The Weapon Of Destruction
- Discussing Day-to-Day Fear | Types Of Fears & How To Overcome Them
- Electromagnetism – Antenna Radiation Patterns | How To Read Antenna Radiation Patterns
- Do Robots Really Have Emotions? | Can Artificial Intelligence Feel Emotions?
- Reduction of Prostaglandin E2
- Increase in blood oxygen concentration
If the connection persists, the condition is called a patent (or persistent) ductus arteriosus (PDA).
In a normal individual, PDA can be thought of as a pathological process which can lead to heart failure but in a patient with TOF, PDA is a life savior.
It provides an alternative route to the lungs so that the volume of deoxygenated blood being oxygenated can be optimized. It’s a sophisticated mechanism which would allow the organs and heart to function at an optimum level.
However, ductus arteriosus is just an alternative to alleviate the signs and symptoms before a much more definitive treatment (surgery) can be performed.
Tetralogy of Fallot is the most common type of cyanotic congenital heart disease. There are a few others which I will write somewhere in the future:
- Transposition of great arteries
- Arterioventricular septal defect
- Tricuspid Atresia
- Hypoplastic left heart syndrome
- Total anomalous pulmonary venous drainage
- Truncus Arteriosus
Now, let’s focus on the management of the Tetraology of Fallot (TOF). Just some information on TOF:

- There are four congenital heart deformities that can be seen in people with Tetralogy of Fallot; ventricular septal defect (VSD), overriding aorta, right ventricular hypertrophy and finally, sub-pulmonic stenosis.
- The severity of symptoms would depend on several factors such as the size of the hole in the VSD, whether or not the ductus arteriosus (a connection between the proximal descending aorta and the pulmonary artery) is present and the degree of the ventricular outlet obstruction (pulmonary stenosis).
- The direction of blood flow will be determined by the pressure gradient inside the respective chamber or blood vessel. For example, when there is a small VSD, blood will flow from the left ventricle to the right and not the other way around; not until the pressure gradient level reverse as a result of certain pathology.
Clinical Presentation

When we are talking about clinical presentation, it’s important to know that, there are a few aspect or information that need to be gathered in order to achieve an accurate provisional diagnosis:
- Patient’s history
- Physical examination
- Provisional diagnosis
- Differential diagnoses
After obtaining all of the above information, finally, we’re ready to proceed to the managing part. Management of a disease can be divided into two which are:
- Investigation
- Treatment modalities
I will talk about management later in the article. For now, let’s focus on the clinical presentation of a patient, how they look like when they were first presented to the clinic/hospital. There are a few signs which indicate a baby is in heart failure. Among all of them, the most important signs to be elicited by a clinician is a heart murmur. Listening to murmur is kinda subjective, it will depend whether or not the clinician in charge has sufficient training or not. Hearing sounds, sometimes, can be deceiving and in paediatric populations, checking heart murmur can be a challenging task (patient often cries especially when they have the stranger or white coat anxiety).
There a few types of heart murmur and all of them correspond to a different kind of heart’s pathology. Refer to the video below to know more.
The age of presentation will depend on the severity of symptoms which would be determined by a few cardiac pathologies. Two of the commonest type of pathologies are:
- A large VSD
- A high degree of right ventricular outlet obstruction
A baby which have one of two of those signs will be presented with cyanosis; blue discolouration of the skin and mucous membrane as a result of a low blood oxygen concentration. If for the sake of argument, the baby presented with both, then they will show symptoms related to hypoxia, a couple months early than the other babies. Parents were usually concerned with the bluish appearances of the baby rather than other symptoms which they might have thought “normal” such as lethargy and irritability.

Clubbing of the finger is a common sign for heart-related diseases but in patients with TOF, they rarely presented with clubbing unless their pathology was detected later in life (if the defect was not severe).
The pathophysiological processes which could lead to the formation of a club finger would take normally around 6 months. Clubbing of the finger is not a specific sign which indicates any type of disease.
They can be found in patients with heart diseases, lung diseases, hyperthyroidism and liver diseases; it signifies that clubbing of the finger is actually a poor indicator of either disease.
Sometimes, people who have clubbing of the finger doesn’t really have anything.
Their exact pathophysiology was not known but it was speculated that clubbing of the finger was caused by interstitial oedema which progresses into an increase of the vascular connective tissue making the finger appears like a club.
Hypercyanotic spell also known as the Tet spell is another condition which could be caused by TOF. If you noticed, some children who have TOF can suddenly become:

- Hyperpnea (increase in deep breathing).
- Irritable
- Prolonged crying
- Cyanosis
If the one who was affected by the hypercyanotic spell is an older child, he/she will know to squat immediately after getting the attack. There are a few reasons why that will cause a temporary fix to the hypercyanotic spell so before going into that, I will explain a little bit more about the pathophysiology of the hypercyanotic spell. There are a few factors which would determine the onset of a hypercyanotic spell:
In several TOF patients especially those with severe pulmonary stenosis, there will be an increase in both of the cardiac output and systemic venous return.
This will cause the pressure of the right ventricle to be higher than the pressure in the left ventricle.
This would cause a reverse flow of blood from the right ventricle into the left ventricle through the VSD due to the pressure difference.
Couple this with a reduced systemic vascular resistance, the cells in the body would be deprived of oxygen which would cause hypoxia.
Low concentration of arterial oxygen along with an increase in the level of carbon dioxide will be detected by the respiratory centre in the brain.
This will cause them to send a signal to a few respiratory muscles to increase the depth and frequency of breathing thus the hyperpnea.
Squatting or putting the affected patient in a knee-to-chest position would allow both the systemic vascular resistance and systemic venous return to decrease, relieving the increase in right ventricle pressure gradient.
It worth noting that, when a child presented with the hypercyanotic spell, they should have been brought for medical consultation for further assessment.
Investigation and Treatment Modalities

When it comes to investigations for TOF, the diagnostic one would be imaging tests.
Well, we can order the standard workup to establish the baseline value such as full blood count (FBC), full blood picture (FBP), renal profile, liver function test and maybe acute phase reactant if the patients came with fever or anything that indicates some kind of inflammation or infection.
An electrocardiogram (ECG) can be performed to check for any sign of right ventricular hypertrophy which can be presented as a right axis deviation. Well, I would not go deeper into the ECG pattern analysis, maybe I will cover it sometime in the future.

Radiological investigations such as a chest X-ray and an echocardiogram can delineate some anatomical abnormalities in the heart structure. The most common finding in the chest X-ray of people with TOF is the boot-shaped heart.
The appearance was caused by a right ventricular hypertrophy which would cause an upward displacement of the apex of the right ventricle coupled with a concave pulmonary artery making it look like a boot.
Before echocardiogram was widely used, cardiac catheterisation was used to check the degree of blockage at the outlet of the right ventricle.
Now, echocardiography has been a gold standard imaging modality to delineate the structural defect of the heart.
Treatment modalities can be divided into two which are conservative and surgical.
Whether or not to proceed with surgical interventions, it will be determined by the severity of the clinical presentation.
The earliest treatment which could be given is prostaglandin.
If you remember, in the introduction part, I did say the importance of keeping the ductus arteriosus open to help reoxygenated any deoxygenated blood which has been pumped through the aorta.
It’s a temporary fix but an effective one.
The bad news is, this kind of treatment is only available if the patient was admitted early (when the ductus arteriosus is not yet closed). Keeping the ductus arteriosus open will provide a constant deoxygenated blood flow to the lungs which would alleviate the hypoxia.
If patients with TOF were suspected to have a hypercyanotic spell, parents should be taught some manoeuvres to fix the problem.
The easiest one would be to put their child in a knee-to-chest position thus making the systemic vascular resistance increase and systemic venous return decrease.
There is some medical intervention that can be given such as:
- Oxygen
- Morphine to alleviate pain and provide a sedative effect
- Bicarbonate to correct acidosis
- Beta-blocker to reduce infundibular spasm

Usually, palliative treatment would be given up until the baby reaches 4-6 months old before corrective surgical options could be discussed. In Malaysia, the most common bypass tube which has been used to improve blood flow into the pulmonary circulation is the modified Blalock-Taussig shunt.
So this shunt would be installed to provide a communication between the subclavian artery and the pulmonary artery.
After the baby has reached the age of 6 months old, a corrective surgery would be done.
There are a few types of corrective surgeries, which I would not mention it here, and if they were performed before the age of 1 year old, the chances of reintervention would be low throughout life and the rate of survival would be up to 85% (to reach 30 years old).
Conclusion
Even though people with TOF are subjected to a life-long follow-up, even after the corrective surgery, their quality of life has been increasing greatly.
It’s important to diagnose this disease as early as we could to yield a good outcome out of all the treatment modalities that are available.
The long-term management will be handled by a paediatrician and a cardiologist.
That’s the much we can take on the topic “The Blue Baby Syndrome | Introduction & Management Of The Tetralogy of Fallot“.
Thanks For Reading
See Other Articles People Are Reading
- Cry Me A River – From Biology To Psychology Of Tears
- Redefining ‘Health’ For The 21st Century | Health Care Changes In The 21st Century
- Missile Technology – The Weapon Of Destruction
- Discussing Day-to-Day Fear | Types Of Fears & How To Overcome Them
- Electromagnetism – Antenna Radiation Patterns | How To Read Antenna Radiation Patterns
- Do Robots Really Have Emotions? | Can Artificial Intelligence Feel Emotions?
Leave a Reply